Every Annual and Open Enrollment Period forces health plans into a balancing act: extremely high call volumes, tight CMS deadlines, and members who often misunderstand required documents. Even highly digitized health plans see significant gaps.
Industry data shows how widespread the problem is:
- 44% of new Medicare Advantage members submit incomplete or incorrect documentation during AEP.
- 28% of Marketplace enrollments require at least one follow-up for documentation .
- Up to 31% of Medicaid renewals fail due to “procedural reasons,” not loss of eligibility .
These gaps create:
- Incorrect or delayed coverage
- Member confusion
- Preventable early-year complaints
- CMS audit risk
Automation helps identify missing documents—but it cannot ensure members truly understand what is required. Assisted member guidance closes the accuracy gap.
The Real Cost of Documentation Errors for Health Plans
| Impact Area | Operational Outcome |
|---|---|
| Incorrect or delayed activation | Higher first-90-day call volume |
| Mismatched eligibility records | Billing disputes & incorrect PCP assignment |
| Incomplete SEP documentation | Compliance exposure |
| Increased manual rework | Backlogs during AEP/OEP |
| Higher grievance/complaint ratios | Stars & CAHPS impact |
CMS reported that documentation inconsistencies remain a top driver of MA complaints.
Where Automation Helps—And Where It Cannot
Digital tools play a key role in modern enrollment and eligibility services:
- Automated reminders
- System flags for missing fields
- Document-upload workflows
- Status tracking through portals
But these systems struggle in four scenarios:
- Low digital literacy
- Complex income or household documentation
- Special Enrollment Period (SEP) nuances
- Non-English-speaking members needing clarification
Assisted Member Guidance: The Missing Link in Clean Enrollment Files
1. Real-Time Clarification Prevents Repeated Errors
Members often confuse “proof of residency” with “mailing address,” or “income verification” with “tax documentation.” A live specialist corrects these misunderstandings instantly.
2. Support for Seniors, Low-Income Families, and First-Time Enrollees
These groups struggle most with document preparation. Assisted support reduces repeat submissions and incomplete files.
3. SEP Documentation Requires Higher Touch
Marriage, relocation, job loss, and other SEP triggers have strict evidentiary rules. Failure to submit correct documentation is one of the top reasons for denied SEP enrollments.
4. Multilingual Engagement Improves Accuracy
Plans serving Spanish, Haitian Creole, Vietnamese, Korean, or Mandarin populations see higher accuracy when clarification is offered in-language.
Hybrid Support Model: Automation + Assisted Guidance
Where automation works
- Tracking submissions
- Sending reminders
- Flagging missing documents
Where assisted guidance adds value
- Explaining exactly which documents qualify
- Helping members understand eligibility rules
- Clarifying household size for Marketplace plans
- Supporting SEP exceptions
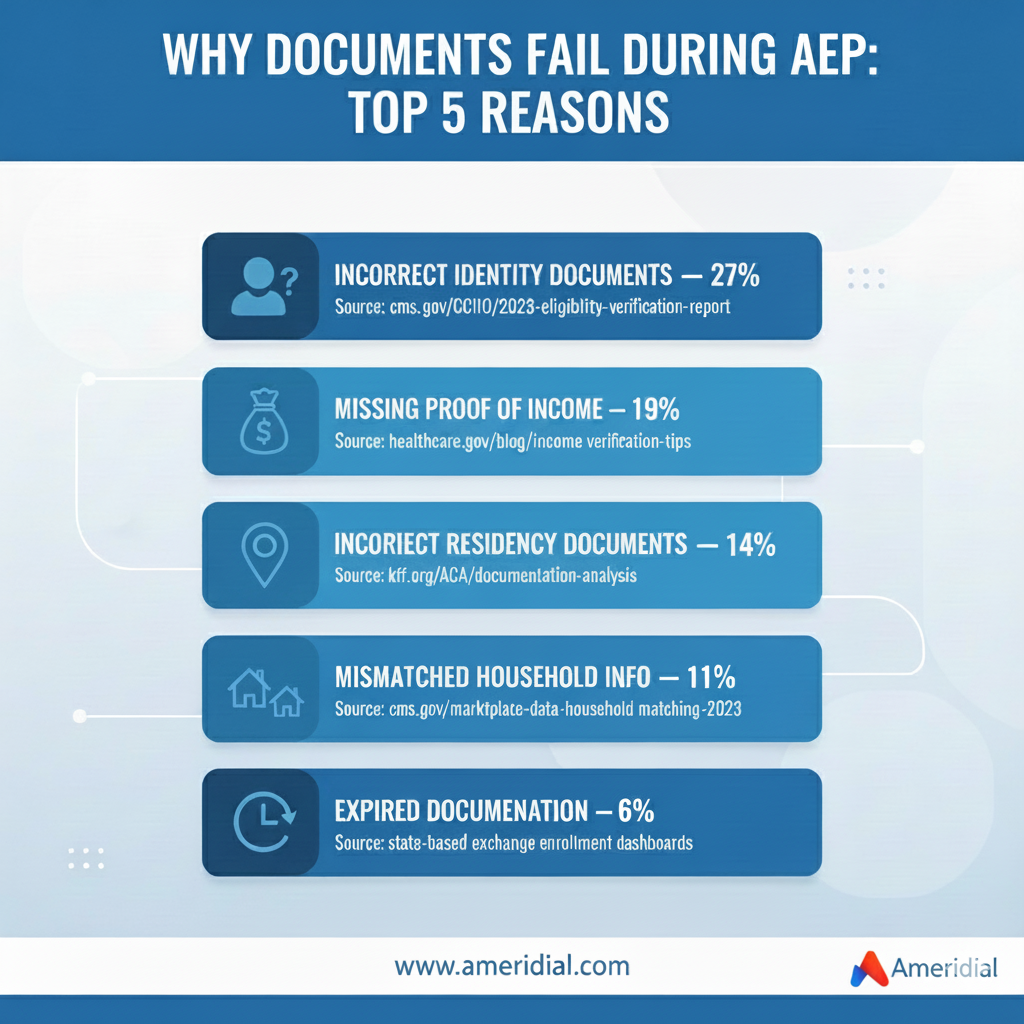
AEP Documentation Gaps
Expected Outcomes for Health Plans
When assisted guidance strengthens digital workflows, plans see:
- 34–40% reduction in incomplete documentation rates (Source: AHIP “Improving Enrollment Experience 2023”).
- Fewer pended applications during AEP
- More accurate eligibility files
- Lower early-year call volume
- Better member satisfaction scores
- Reduced CMS complaints & audit exposure
How Ameridial Strengthens Enrollment & Eligibility Workflows
- Assisted document guidance for residency, income, identity, and household requirements
- Hybrid digital + agent workflows for speed and accuracy
- Multilingual support for Marketplace, Medicaid, and MA populations
- AI-QMS monitoring for 100% quality and compliance
- Surge-ready staffing to support AEP/OEP volumes
Documentation gaps aren’t a technical problem—they’re a clarity problem. When health plans combine efficient digital tools with guided member assistance, the result is a smoother, more accurate enrollment cycle and a significantly lower risk of CMS escalation.
Ready to reduce enrollment errors and strengthen eligibility accuracy?
Our Ameridial experts are here to help you build a more compliant, precise, and scalable enrollment operation.




